Additional Vital Signs: Pulse & SpO2
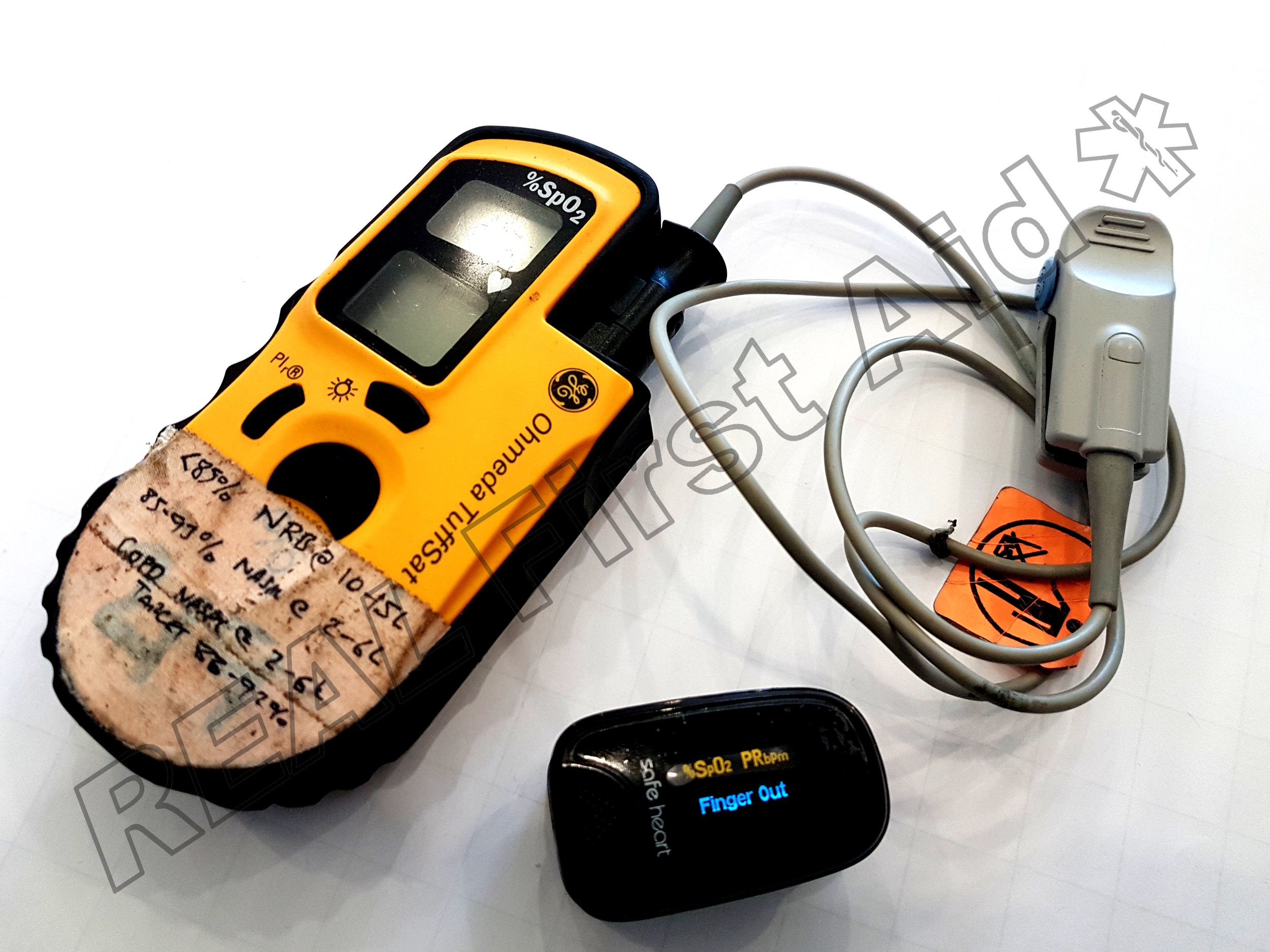
In addition to the 5 Basic Vital Signs we can add Pulse and Sp02 (Oxygen Saturation), but to do this we require equipment; the Pulse Oximeter.
Pulse
Checking a pulse is hard. On a fit, healthy casualty in low stress situations it can sometimes be easy to feel a nice juicy pulse but in reality, with a poorly casualty, and you’re having a bit of a moment and you are not in a nice, quiet training environment, don’t bother.
In the late 90’s several studies were conducted to assess the accuracy of lay people (1), First Aiders, Paramedics and even Doctors in assessing simply the presence of a pulse. In one study, success rates were as low as 45% in identifying the presence of a pulse (2) and in another, junior doctors took an average of 18 seconds to identify a pulse (3).
It was for these reasons that, based on advice from the International Liaison Committee on Resuscitation, the United Kingdom Resuscitation Council and American Heart Association removed routinely checking for a pulse as a sign of life from First Aid training in the 2000 updates.
But checking a pulse does have value – as with all of the basic vital signs, knowing whether the casualty’s pulse rate is within a normal range can assure us; if the casualty’s pulse is outside of these ranges it can even point us toward a particular problem.
If someone has been running around we would expect their pulse to rise. We’d also expect them to be hot, red and breathing faster.
If they haven’t been running around, but they’re hot, red, fast breathing and with a fast pulse, we may have a problem, this could indicate sepsis.
If they’re a trauma casualty; hot, red and with a slow, strong pulse, this could indicate internal head injury.
If they’re a trauma casualty, cold and pale with a fast pulse, this could be hypovolaemic shock.
Just don’t bother trying to check it manually. We’re going to use the Pulse Oximiter: The Pulse Oximeter is a small diagnostic tool which is predominantly used to identify the casualty’s oxygen saturations but it will also show the casualty’s pulse. With one of these, we don’t need to be wasting time reaching around the casualty, desperately feeling for a pulse.
| Age | Normal Pulse Rate |
|---|---|
| Neonate ( <28 days ) | 100-205 |
| Infant ( 1 month - 1 year ) | 100-190 |
| Toddler ( 1-2 years ) | 98-140 |
| Pre-school ( 2-5 years ) | 80-120 |
| 6-11 years | 75-118 |
| 12 years - adult | 60-100 |
| Athlete | 40-60 |
| Pulse | Possible cause |
|---|---|
| Rapid, regular and full | Exertion, fear, fever, hypertension |
| Rapid, regular and weak | Hypovolaemic shock |
| Slow | Head injury, drug use, poisons, cardiac problems |
| Irregular | This is quite common and not necessarily a problem. |
Pulse Oximetry
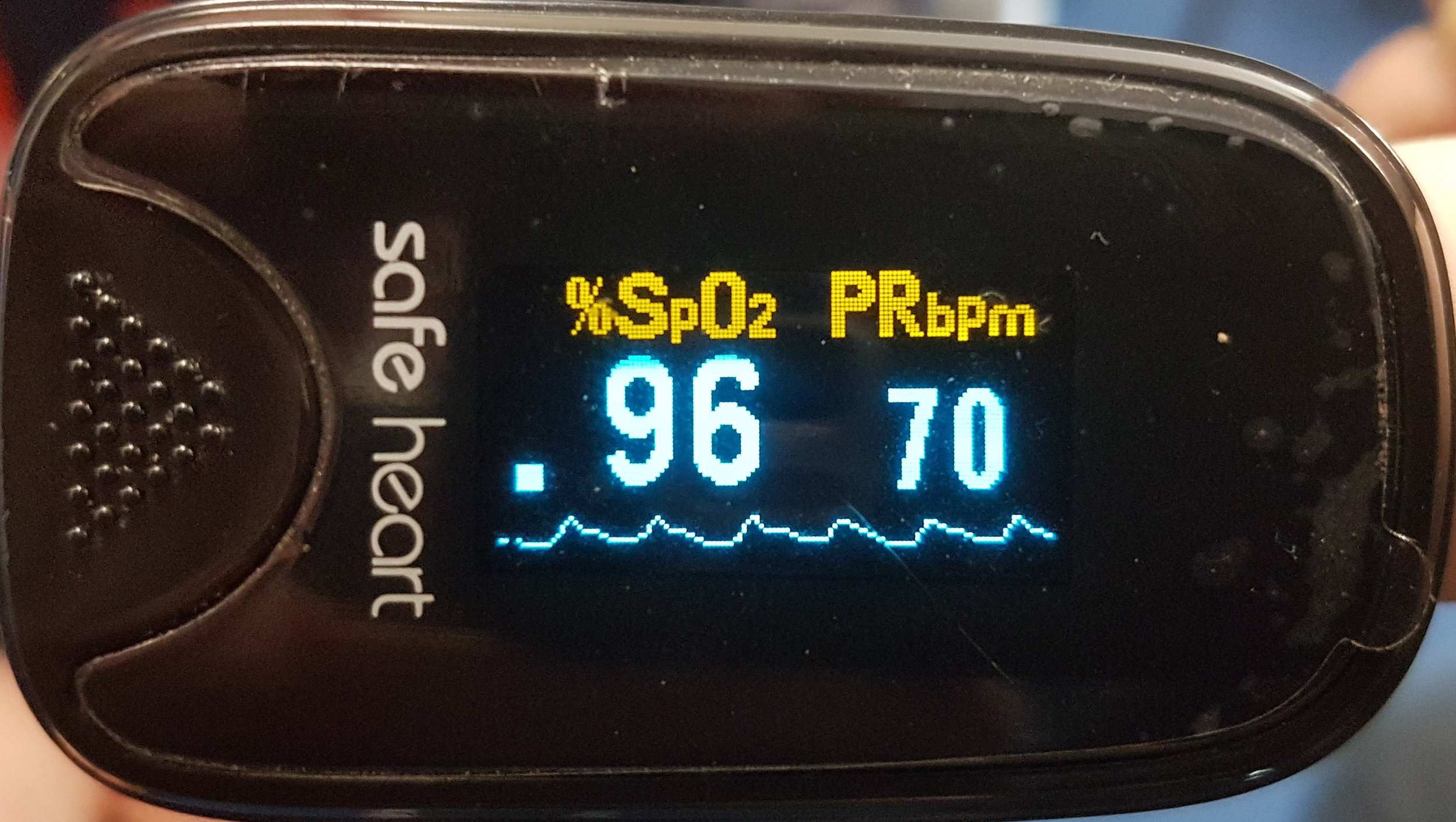
Pulse oximetry measures the amount of oxygen being carried in your blood, as a percentage. The measurement is taken at the finger using a Pulse Oximeter. This measurement is known as the Sp02 – the saturation of peripheral oxygen – and it is an estimate of the Sa02 – the saturations of arterial oxygen.
The haemoglobin in your red blood cells carry the oxygen (with a small amount being dissolved in the blood). Each Haemoglobin molecule can carry 4 oxygen molecules. If all of your haemoglobin have four oxygen molecules bound to them, your blood would be 'saturated' with oxygen and you would have an SpO2 of 100%.
Most people don’t have oxygen saturations of 100% so a range of 95-99% is considered normal.
Anything below 95% is an indicator of hypoxia – a lack of oxygen perfusing the tissues.
A reduction in SpO2 is the most reliable sign of hypoxia in a casualty; cyanosis and other clinical signs are difficult to detect and often late in presenting (4-6). Increased breathing rate is associated with hypoxia but, again, the evidence suggests that this link is not strong enough (or even present in all cases) to rely on as a sign of hypoxia. (7-9).
The pulse oximeter is a rapid diagnostic tool that allows you to measure and monitor the casualty’s oxygenation levels. Knowing the casualty’s Sp02 will also allow you to give an appropriate amount of oxygen if that is within your skillset.
A reduction of 3% or more SpO2, even if within normal saturations, is an indicator to performing fuller assessment of the patient (and the oximeter signal) because this may be the first evidence of an acute illness (10).
| Casualty | SpO2 |
|---|---|
| Normal - Healthy | ≥ 94% |
| Normal - COPD | 88% - 92% |
| Hypoxic | 85% - 93% |
| Severely Hypoxic | < 85% |
Limitations
Poor peripheral circulation and hypothermia are the most common cause of false low readings
Movement – including shivering - and poor placement can also affect the reading.
Black, Blue and Green nail varnish can present inaccurate readings. Acrylic nails do not appear to interfere. (11)
Bright lights, especially fluorescent lights can affect the readings. (12)
Carbon Monoxide has an affinity to haemoglobin 210 greater than oxygen; as such a casualty with Carbon Monoxide poisoning may show falsely high Sp02 readings as the Pulse Oximiter interprets the heamoglobin to be saturated with oxygen when they are saturated with Carbon Monoxide.(13)
Pulse Oximeter on a healthy female at rest….wearing blue, glitter nail gels.
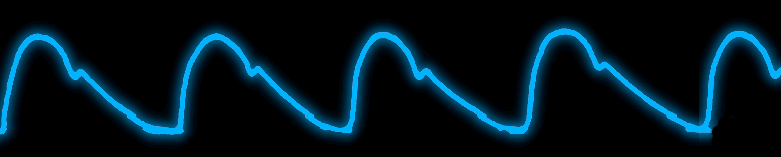
The Waveform
As well as the pulse and oxygen saturations, the third piece of information we can look at is the waveform. This undulating waveform is representative of the casualty’s blood pressure – peaking at the systolic pressure (the contraction of the heart) and dropping to the diastolic pressure. While the pulse oximeter does not measure blood pressure nor give numerical values, this visual display can present a graphic indication of the quality of their pulse.
A regular, repetitive waveform with obvious peaks and troughs is indicative of a good quality peripheral perfusion.
A particular feature of the cardiac cycle waveform is the “dicrotic notch”. This notch on the descending side of the waveform indicates the closing of the aortic valve and the end of the systolic phase – the pulse. It is speculated that the position of the notch can indicate vasomotor control – it appears the dicrotic notch descends towards the baseline during vasodilation and ascends towards the peak during vasoconstriction. (14)
A shallow, weak waveform would mean there is poor peripheral perfusion which could could indicate poor cardiac output or simply the casualty does not have great circulation in their fingers. An exaggerated notch in addition to a low waveform is indicative of poor cardiac output (15).
Normal waveform
Strong, regular, steep ascending and shallow descending waveform with a noticeable dicrotic notch.
Small, weak waveform
| Waveform | Physiological causes | Possible disease |
|---|---|---|
| Small and weak | Decreased stroke volume, Increased peripheral resistance | Heart failure, hypovolaemia |
Large and bounding
| Waveform | Physiological causes | Possible disease |
|---|---|---|
| Large and bounding | Increased stroke volume, Decreased peripheral resistance. | Fever, anaemia, aortic regurgitation, traumatic brain injury |
Pulsus alternanse
| Waveform | Physiological causes | Possible disease |
|---|---|---|
| Pulse alternanse | Pulse amplitudes alternates | Left ventricular failure |
No dicrotic notch
| Waveform | Physiological causes | Possible disease |
|---|---|---|
| No dicrotic notch | Increased arterial resistance | Coronary heart diseases |
Chaotic
| Waveform | Physiological causes | Possible disease |
|---|---|---|
| Chaotic | Usually Arrhythmia or motion artefact | Possibly an arrhythmia such as Ventricular Tachycardia, Ventricular Fibrillation but more commonly background movement. Espeically is your casualty is not looking quite happy. |
Examples
Strong waveform with good dicrotic notch indicating good pulse pressure and perfusion.
Strong pulse pressure but without an obvious dicrotic notch indicating good pulse pressure and perfusion but increased arterial resistance.
Weaker waveform but with noticeable dicrotic notch indicating lower blood pressure but normal vascular resistance.
A pulse oximeter is not necessarily the most accurate diagnostic tool but is an essential item for the remote medic:
Finding a pulse manually is hard enough, especially when you are flapping (16-25) to the point that a manual check for pulse was removed from the requirements of the lay-responder and de-emphasized for the requirements of healthcare professionals from resuscitation guidelines back in 2010.
If a pulse can be detected manually, determining strength and regularity is even harder, especially if the casualty is poorly perfused. The pulse rate is just one aspect but the waveform is really useful as a pictorial representation of strength and regularity of the casualty's pulse.
Pulse in isolation is not a particularly useful vital sign - how the casualty appears will tell you more but with more information your picture is not necessarily different but 'higher definition'. Having more information can help confirm or challenge your diagnosis or decision making.
A poorly perfusing casualty will be obvious before the Sp02 drops but....if you can quantify it you can see the rate of change. A 3% drop in SpO2 is a cause for concern but what does that look like in terms of colour or Level of Response? What does that look like on a casualty with a dark skin tone?
If you don't carry oxygen why carry a pulse oximeter? You may have O2 available e.g. onboard an aircraft or at a swimming pool. I bet they don't have a pulse oximeter.
Some people just need reassurance. I have put a pulse oximeter on many 'casualties' who are just a little upset; you've introduced a bit of esoteric kit which makes the casualty think 'this person knows what they're doing'. Give it a hard stare, look reassuringly at the casualty and say "This is fine...you're going to be OK". Sometimes this is all people need. An arm around their shoulder, tea and cuddles.
For the size and weight, why not. My EDC does not contain bandages and tourniquets (unless the Needs Assessment determines otherwise) because with decent scissors I have all the bandages I need. I don't carry a full med bag everywhere because there isn't the need but at less than £20.00 and about the size of two boxes of matches there is no reason not to have one.
Next Article: Blood Pressure
References
Bahr J, Klingler H, Panzer W, Rode H, Kettler D. (1997) “Skills of lay people in checking the carotid pulse”. Resuscitation 35:1, 23–26
Eberle B, Dick WF, Schneider T, Wisser G, Doetsch S, Tzanova I. (1996) “Checking the carotid pulse check: Diagnostic accuracy of first responders in patients with and without a pulse”. Resuscitation 33: 107–116.
Flesche CW, Breuer S, Mandel LP, Breivik H, Tarnow J. (1994) “The ability of health professionals to check the carotid pulse”. Circulation. 90 (Suppl I): 288
World Health Organisation(2011) Pulse oximetry training manual. ISBN 978 92 4 150113 2
Jubran, A. (1999) “Pulse oximetry”. Critical Care 3:R11
Jubran, A. (1999) “Pulse oximetry”. Critical Care 19:272
Mower WR, Sachs C, Nicklin EL, Safa P, Baraff LJ. (1996) “A comparison of pulse oximetry and respiratory rate in patient screening”. Respiratory Medicine. 90: 593-599.
Berman S, Shanks MB, Feiten D, Horgan G, Rumack C. (1990) “Acute respiratory infections during the first three months of life: clinical, radiographic and physiologic predictors of etiology”. Pediatric Emergency Care. 6: 179-182.
Cherian T, John TJ, Simoes E, Steinhoff MC, John M. (1988) “Evaluation of simple clinical signs for the diagnosis of acute lower respiratory tract infection”. Lancet. 8603: 125-128.
O’Driscoll BR. Howard LS. et al(2017) “BTS guideline for oxygen use in adults in healthcare and emergency settings”, Thorax, Volume 72 Supplement 1 Pages i1–i90
Cote CJ, Goldstein EA, Fuchsman WH, Hoaglin DC. (1989) “The effect of nail polish on pulse oximetry”. Anesthesia & Analgesia. 67: 683-686.
Amar D, Neidzwski J, Wald A, Finck AD. (1989) “Fluorescent light interferes with pulse oximetry”. Journal of Clinical Monitoring. 5: 135-136.
Blumenthal I. (2001) "Carbon Monoxide Poisoning". Journal of the Royal Society of Medicine. v.94(6)
Murray WB, Foster PA. (1996) “The peripheral pulse wave: information overlooked”. Journal of Clinical Monitoring. Sep; 12(5):365-77.
D Smith and E Craige. (1986) “Mechanism of the dicrotic pulse”. British Heart Journal. Dec; 56(6): 531–534.
Bahr J, Klingler H, Panzer W, Rode H, Kettler D. (1997) “Skills of lay people in checking the carotid pulse”. Resuscitation. 35:23–26.
Brennan RT, Braslow A. (1998) “Skill mastery in public CPR classes”. American Journal of Emergency Medicine. 16:653–657.
Chamberlain D, Smith A, Woollard M, Colquhoun M, Handley AJ, Leaves S, Kern KB. (2002) “Trials of teaching methods in basic life support : comparison of simulated CPR performance after first training and at 6 months, with a note on the value of re-training”. Resuscitation. 53:179–187.
Eberle B, Dick WF, Schneider T, Wisser G, Doetsch S, Tzanova I. (1996) “Checking the carotid pulse check: diagnostic accuracy of first responders in patients with and without a pulse”. Resuscitation. 33:107–116.
Frederick K, Bixby E, Orzel MN, Stewart-Brown S, Willett K. (2002) “Will changing the emphasis from ‘pulseless’ to ‘no signs of circulation’ improve the recall scores for effective life support skills in children?” Resuscitation. 55:255–261.
Lapostolle F, Le Toumelin P, Agostinucci JM, Catineau J, Adnet F. (2004) “Basic cardiac life support providers checking the carotid pulse: performance, degree of conviction, and influencing factors”. Academic Emergency Medicine. 11:878–880.
Moule P. (2000) “Checking the carotid pulse: diagnostic accuracy in students of the healthcare professions”. Resuscitation. 44:195–201.
Nyman J, Sihvonen M. (2000) “Cardiopulmonary resuscitation skills in nurses and nursing students”. Resuscitation. 47:179–184.
Owen CJ, Wyllie JP. (2004) “Determination of heart rate in the baby at birth”. Resuscitation. 60:213–217.
Sarti A, Savron F, Ronfani L, Pelizzo G, Barbi E. (2006) “Comparison of three sites to check the pulse and count heart rate in hypotensive infants”. Paediatric Anaesthesia. 2006; 16:394–398.